According to Cleveland Clinic, a female fetus comprises about 106 to 2×106 oocytes in the ovaries at birth. In simple terms, oocytes are immature eggs in the female reproductive system. Surprisingly, that is all the eggs the female will ever produce.
At puberty, the remaining number of eggs is about 300,000 in total. During the reproductive lifetime of that woman, about 0.1% of those eggs will be ovulated(1).
Also, the Centers for Disease Control and Prevention (CDC) say that a woman is bound to experience ovulation during her lifetime which is signified by the discharge of blood at any interval between 24 to 32 days(2). The monthly blood discharge is renowned as predictable periods.
However, the monthly discharge is always in preparation for the likelihood of conception. Before a cycle can occur, there some hormones have to work in unison(3). Without hormones, the menstrual cycle may not achieve completion because the hormones are responsible for the maturity and release of the ovum or egg.(4)These hormones are:
- Sex hormones – estrogen and progesterone
- Follicle-stimulating hormone
- Luteinizing hormone
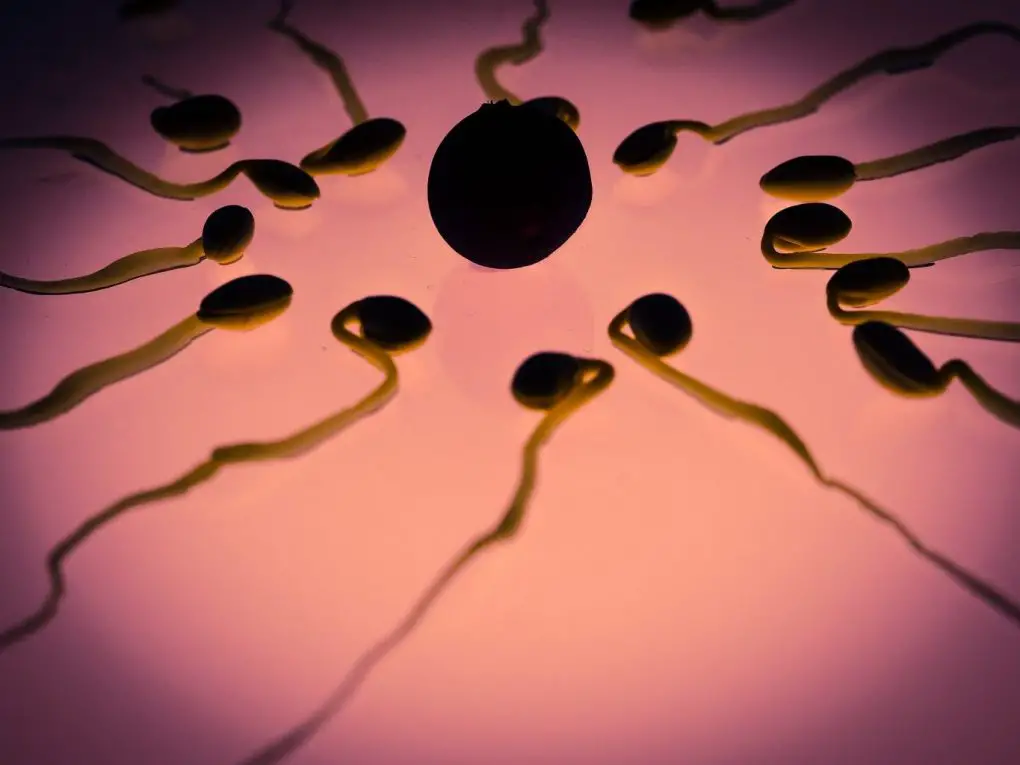
When a man and woman copulate, the man releases sperm cells. During this period, the woman’s ovary releases a mature egg which makes it way to the Fallopian tube. The merging of the sperm cell with the egg gives rise to fertilization.
According to the Mayo Clinic, fertilization doesn’t occur immediately after sexual intercourse – the sperm can survive up to 3 to 5 days within the reproductive tract of the woman.(5). Once fertilization of the egg occurs, it travels to the womb or uterus. Afterward, a fetus develops when the fertilized egg attaches itself to the uterus’ lining.(6)
However, the uterus has to prepare for the reception of the fertilized egg. For that reason, the thickness of the wall of the uterus must increase during ovulation. Without fertilization, menstrual flow occurs when this lining is shed after 14 days. Meanwhile, ovulation is not always characterized by monthly periods.
Whenever the ovary releases a ripe egg, the lower abdomen contracts repeatedly. Some other women lose blood instead. Both phenomena are indicators of ovulation.
It is mostly a misconception that menstrual cycles or menstruation is an indication of ovulation whereas the case may not be so. The buildup of the uterus’ lining is the ovulatory cycle. Due to the production of estrogen, many women experience the ovulatory cycle.
According to Dr. Mary Jane Minkin, a woman bleeds very heavily when the buildup gets to a particular threshold and the lining casts off. In the meantime, the production of progesterone occurs during ovulation which counteracts the high volume of blood to generate a better-controlled bleeding.
Classification of Ovulation
The general misconception that ovulation takes place after two weeks of the most recent period is absurd. Ovulation depends on the woman; therefore you should expect different timing and duration for the cycle. For instance, the American Society for Reproduction Medicine classifies woman based on their menstrual cycles as following:
- 28-day menstrual cycles – A woman who ovulates between 13 to 15 days has this form of menstrual cycle
- 27 to 34 days menstrual cycles – A woman who ovulate between 13 to 20 days has this form of menstrual cycle.(7)
Clues and timing for ovulation
A professional obstetrician also claims that many women do not pay cognizance to their ovulation timing and periods. There are many telltale signs that a woman may be ovulating if it is too much stress to note the timing on a notepad or a calendar.

Basal Body Temperature
There are likely changes that will occur in the basal body temperature of a woman before ovulation. A woman can keep track of these changes by noting the basal body temperature. By definition, the basal body temperature is the temperature of the woman in the morning while in bed. Hence, a woman can predict her fertility if she can record the changes for about two to three cycles. The early morning body temperature may increase by about 10F (-17.220C) after ovulation. And Mayo Clinic also buttresses the fact that fertility is at its peak at a certain period about 48 to 72 hours before the increase in temperature.(8)
Vaginal Secretions
The most cliché sign that ovulation is a few days away is changes in vaginal secretions. These secretions are characterized by stretchy, clear, thin, and slippery mucus from the cervix before ovulation.
While it takes place a few days before ovulation, it will interest you to know that the lower part of the uterus is the cervix. Nonetheless, this is a clear signal for the commencement of ovulation and the release of an egg from the ovaries.
The thin and clear mucus increases in turgidity to become thick and cloudy on the second day after ovulation. Many women hardly pay attention to the changes in the cervical fluid but it is great you know this now.
Luteinizing Hormone
The rise in the luteinizing hormone occurs about 24 to 36 hours before ovulation. A classic sign for the release of an egg from the ovary is the rise in luteinizing hormone. If you want to detect the hormonal increase, you can purchase an ovulation predictor kit.
How does the kit work? All you need to do is to dip the kit in your urine sample in the days before the ovulation cycle. The test shows a positive result when it detects an increase in the luteinizing hormone.
Fertile Window
Even though pregnancy is synonymous to women, such a woman has to be fertile enough to conceive. Basically, fertility occurs in selected parts of the monthly cycle. The periods, according to numerous literature, are 6 days in total – the ovulation day and the 5 days before it.
The American Society for Reproductive Medicine strongly supports the claim. Also, these studies prove that pregnancy occurs from sexual intercourse within three days before and on the ovulation day.(9)
In a recent study to determine the likelihood that the six fertile days are within the menstrual cycle, the results were shocking. A total of 221 women who were planning conception and had discontinued birth control pills and methods were used in the study.
The women supplied the usual length of their cycles and the regularity of their cycles before the experiment. Every day, during the experiment, the women will collect their first urine sample of the day. In addition, they also monitored and recorded the days of menstrual bleeding and sexual intercourse.(10)
The results showed that the fertile window has no defined days of occurrence within the menstrual cycle. Between 6 to 21 days, there was about 10% likelihood that a woman was in a fertile window.
Since late ovulations are seemingly sporadic, no woman could predict its occurrence – about 4 to 6% of women with sporadic late ovulation cycles were fertile in Week 5 of the menstrual cycle.
Hence, the number suggests that about 30% of women experience their fertile window according to suggestions from numerous studies. While some women are late bloomers in the fertility department, other women reach their fertility window earlier.
Therefore, do not mistake regular cycles for a consistent fertility window period; it is highly unpredictable in most women.(11)
Repeated Ovulation within a Month
Canadian researchers from the University of Saskatchewan are of the opinion that ovulation may take place more than once within a period of 30 days. The research also explains why pregnancy occurs in women who ingest hormonal contraceptives – this is due to the fluctuations in the rhythm period of contraception.
The study involved about 63 women – a combination of nulliparous women and women with children – with regular menstrual cycles. The initial theory was that about 15 to 20 follicles will grow at the start of the menstrual cycle.
Meanwhile, only one of the follicles becomes a mature egg towards mid-cycle. But in this experiment, all the women had a follicular development of at least two waves. The consistency of ovulation in these women is still a mystery as current scanning techniques cannot detect the smaller egg except the follicles.
The Director of the Reproductive Biology Research Unity and the Team Lead of the study, Dr. Roger Pierson, said that about 40% of the subjects could have unpredictable ovulation periods because of the high potential of production of more eggs than one.
The result came as a shock because it would mean that most textbooks about ovulation would be adjusted to suit the new theory.
Pierson boosted his facts by explaining that the fluctuations may support the:
- Failure of natural family planning
- Periodic failure of hormonal contraception
- Different conception dates of fraternal twins
More so, the results are a leeway to assisted reproduction and contraception. In a particular month, many women who opt for in vitro fertilization may have more oocytes for harvest.
Sometimes, the monthly intake of oral contraceptives intersects a week of the intake of placebo pills. These findings question the basis for such an act. At the Hammersmith Hospital in London, the Reproductive Medicine Head – Professor Robert Winston – supports the findings stating them as ‘logical and expected’. (12)
Ovulation Test in The Home
If a woman does not ovulate, she may not conceive even when she experiences a monthly flow. For this reason, ovulation predictor kits are perfect tools to determine the occurrence or absence of ovulation.
Sold across numerous pharmacies and drug stores, the kit tests for the increase in luteinizing hormone in the urine sample of the woman. Again, Mayo Clinic states that the increase in the hormonal discharge takes place within the window period of 24 to 36 hours before ovulation.
Nevertheless, the March of Dimes suggests that the most appropriate time to use the kit is 10 days after the first day of the previous period.
Minkin also recommends a visit to the gynecologist when the test shows a negative result because the stimulation of ovulation is somewhat simple. There are several methods of initiating ovulation such as prescribing drugs that stimulate the ovaries to prepare for the release of an egg – and this method does not depend on the irregularity or absence of ovulation.
Ovulation Problems
The ovulation problem is not a death sentence because they are several reasons that may give birth to the condition. According to the United States Department of Health and Human Services, for instance, a blocked fallopian tube in some women may be due to:
- Surgery for an ectopic pregnancy or endometriosis
- Pelvic inflammatory disease
Also, the American College of Obstetricians and Gynecologists reveal that ovulation may be absent or irregular due to an abnormality in the hormonal level or concentration.(13)
An example is Polycystic Ovary Syndrome (PCOS) which occurs to the abnormality of some hormones or the irregularity or absence of the menstrual cycle. Meanwhile, ovaries have a low probability to release eggs in the presence of thyroid problems.
 The American Society for Reproductive Medicine also suggests that women with a BMI(Body Mass Index) of 18.5 or less are underweight and may be victims of irregular menstrual cycles.(14)In worst case scenarios, ovulation may cease completely.
The American Society for Reproductive Medicine also suggests that women with a BMI(Body Mass Index) of 18.5 or less are underweight and may be victims of irregular menstrual cycles.(14)In worst case scenarios, ovulation may cease completely.
On the other hand, BMI greater than 18.5 may be obese and experience irregular ovulation and irregular periods. Furthermore, excessive exercise and stress are huge factors that affect the timing of ovulation. According to Mayo Clinic (15), there are two instances under which ovulation disorder may occur:
- Intense physical stress may cause a delay in ovulation
- Physical or emotional stress may prevent or delay ovulation
According to the Center for Disease Control (CDC) and the U.S. Department of Health and Human Services infertility may be associated with ovulation problems. More so, it plagues about 12% of individuals within the age group of 15 to 44.(16)
The literature on Ovulation Disorder
Also known as the menstrual disturbance, ovulation disorders are generating global concerns in about 25% of women seeking conception. According to the World Health Organization, there are three categories of couples with ovulation disorders.
- Group I disorders – About 10% of women with ovulation disorder is due to hypothalamic-pituitary insufficiency. This group includes serious conditions such as hypogonadotropic hypogonadism and hypothalamic amenorrhea. A woman with amenorrhoea has a deficiency in estrogen and low gonadotrophins.
- Group II ovulation disorders – About 85% of women with ovulation disorders belong in this group and the condition is due to malfunction of the hypothalamic-pituitary-ovarian axis. The group includes hyperprolactinaemic amenorrhoea and syndrome of polycystic ovary.
- Group II ovulation disorders – About 5% of women with ovulation problems belong in this group and the condition I due to ovarian failure.
For the purpose of this article, we shall consider the first two types of ovulation disorder. The reason is that the last group requires an intense solution such as IVF treatment and oocyte donation – solutions that require a broad scope of knowledge and literature.
Nevertheless, Group I and Group II problems require immediate and available solutions such as modifications in lifestyle, drug treatment, and surgical intervention.
Group I
Hypogonadotropic hypogonadism is the first class of ovulation disorders that is a result of a hypothalamic-pituitary failure. This group includes serious conditions such as hypothalamic amenorrhea.
A woman with amenorrhoea has a deficiency in estrogen and low gonadotrophins. There is no certain cause for hypogonadotropic hypogonadism. But studies suggest that the condition may be innate. For instance, a condition known as Kallmann’s Syndrome by association with anosmia.
Excessive exercise and low body weight are offshoots of hypothalamic amenorrhea. As most causes of infertility, hypopituitarism is rare. Thus, ovulation induction should not be considered except the condition is investigated with great intent.
Depending on the diagnosis, the treatment of this group of ovulation disorder is possible. Some options to consider include:
- Normalization of weight and exercise – this solution is also known as a lifestyle intervention
- Pulsatile gonadotrophin-releasing hormone
- Human menopausal gonadotrophin
Group II ovulation disorders
About 5 to 10% of women around the world are plagued with the problem of polycystic ovary syndrome (PCOS). The problem belongs in the heterogeneous group of disorders. Interestingly, it is the most common group of ovulation disorder among women within the reproductive age. Some characteristic of PCOS may include:
- Obesity and hyperandrogenism
- Anovulatory infertility
- Oligo- or amenorrhoea
The pathogenesis of the disorder depends largely on insulin resistance. From an ultrasound examination of the ovaries, there are multiple small antral follicles with characteristic features.
The Rotterdam consensus, in 2003, chose a definition for PCOS. By their definition, PCOS occurs in the absence of the causes of menstrual disorder or excess of androgen and in the presence of at least two of the following conditions:
- Polycystic ovaries on ultrasound scan
- Hyperandrogenism (clinical and/or biochemical)
- Oligo-ovulation and/or anovulation
Possible treatments for the condition are:
- Medical treatment
- Weight loss
- Assisted conception (usually in vitro fertilization (IVF))
- Second-line treatments including laparoscopic ovarian diathermy (LOD) and injectable gonadotrophin ovulation induction
Because of the relationship between exacerbation of PCOS and increased insulin resistance as determinants of obesity, the first line of treating obese PCOS patients is weight loss. (17)
P.S. If you find this post useful and interesting, please do not hesitate to share it.
If you have something to add- Leave a comment below!
Leave a Reply